HALIFAX, NS - Dr. Simon Sherry says Nova Scotia has to get serious about suicide prevention.
“We need real actions with real funds and real deadlines,” the Halifax-based clinical psychologist said in an interview Sept. 7. “Now we have a largely unco-ordinated approach, we have an out-of-date approach. When you go to the province’s suicide prevention website , there are seven links, three of them are broken and inoperable.”
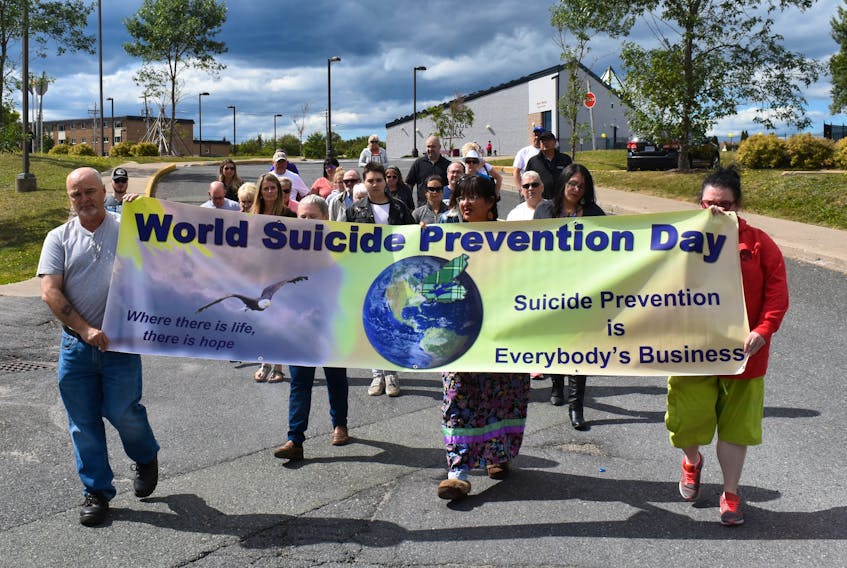
In a news release last week ahead of Suicide Prevention Day Sept. 10, Sherry issued a call for a new suicide prevention strategy in Nova Scotia. It was sparked by his experiences as mental health care provider in Nova Scotia and an alarming rise in suicides in the province in recent years.
According to Statistics Canada, there were 134 suicides in Nova Scotia in 2016, compared to 2000 when there were 75 deaths.
“Between the years of 2000 and 2012, Nova Scotia’s suicide rate increased more than any other province in Canada,” Sherry said. “Over that time period, we went from being a province that in comparison to the national average had a below-average suicide rate to a province that now in comparison to the national average has an above-average suicide rate.
“Why? Part of any provincial suicide prevention strategy should be very careful surveillance of the population. We should be tracking and understanding the trends within our population when it comes to suicide. We do not have a nuanced understanding of what’s driving these increases.”
ALSO SEE:
EDITORIAL: SUICIDE PREVENTION DOESN’T JUST TAKE A DAY
‘HE OWNED ME’: KINGS COUNTY WOMAN TALKS ESCAPING HUMAN TRAFFICKING IN TORONTO
NEW PROVINCIAL SEXUAL VIOLENCE STRATEGY UNVEILED IN KENTVILLE
Nova Scotia’s suicide prevention strategy, based on research done in 2004, is badly outdated, he said, pointing to Quebec, which dedicates $700,000 per year to suicide prevention, as an example of how government action can make a difference.
“In 1998, they had an alarmingly high suicide rate, much higher than any other province in Canada and they started putting specific funds to accomplish specific tasks by specific deadlines into a suicide prevention program,” Sherry said. “They dropped their suicide rate by 30 per cent overall and, most impressively, by 50 per cent in youth.”
Quebec followed World Health Organization protocols to provide education, train additional professionals and make a public commitment to reduce suicide, said Sherry, who’s also a professor in the Department of Psychology and Neuroscience at Dalhousie University.
Suicide prevention advocate Laurel Walker said Sherry is “right on the money” about the need for better funding and improved access to services.
Walker has struggled with depression and anxiety since she was a teenager. She had to leave the province to receive treatment for acute stress disorder, which was sparked by the suicide of a woman she was helping as a mental health peer counsellor in 2012.
“It’s very difficult to get the help that you need when you need it,” said Walker, who along with her friend Fran Morrison, whose son took his own life in 2011, heads the group #HowManyNSHA-IWK.
“Our system is built around Band-aid solutions and only treating the worst when they have to go to the ER and they’re really in crisis,” Walker said. “If we had things set up, preventative measures, when someone reaches out the first time, their calls would not be ignored, they would be pointed in the right direction.”
Sherry said the health system particularly needs to do a better job in working with vulnerable groups such as people with schizophrenia, bipolar disorder and severe depression, who are “at ultra-high risk” to engage in suicidal behaviour.
“We need to make more accessible psychotherapy and medications that will combat those forms of mental illness.”